Background
Spinal dural arteriovenous fistulas (sDAVFs) are one of the treatable causes of myelopathy, resulting from venous hypertension, cord edema, and resultant ischemia. Steroids might induce abrupt neurological deterioration, presumably due to an increase in venous hypertension. Materials and Methods: A total of 62 consecutive type-1 sDAVF patients between January 2001 and January 2020 were included in the study. All patients received perioperative steroids (dexamethasone – 0.5 mg/kg/day divided into four doses) beginning the day before surgery and continued for 3 days postoperatively. The clinical presentation, imaging findings, acute preoperative neurological deterioration, and its relationship to the timing of intravenous steroids and surgical outcomes were analyzed. Results: A total of 7/62 sDAVF patients (11.3%) experienced acute neurological deterioration. All seven patients were male with a mean age of 54.7 years ± 12.5. Progressive myelopathy was the most common clinical syndrome at presentation (93.4%). In all but one of these seven patients, the most recent clinical follow-up indicated disease stability, with symptoms either improving or remaining unchanged from the pre-interventional status. Univariate analysis revealed that none of the prognostic markers (age, gender, duration of symptoms, fistula location, and length of cord edema) were statistically significant between the individuals who worsened after steroid therapy and those who did not. The overall mean Nurick recovery rate (NRR) was better in the cohort with acute worsening after steroid therapy (46%) as compared to an NRR of 19.4% in those without acute worsening. Conclusion: Acute preoperative neurological impairments following steroid administration are transitory when treated promptly with surgical intervention and have little influence on long-term functional results after arteriovenous fistulae disconnection.
INTRODUCTION
Spinal dural arteriovenous fistulas (sDAVFs) are the most common spinal vascular disorder and treatable causes of progressive myelopathy.[1] They are increasingly being reported in the advent of advances in spinal neuroimaging.[2] Venous hypertension secondary to the arteriovenous (AV) fistula is the probable pathophysiological mechanism leading to neurological deficits. Several factors are known to exacerbate this condition, including physical straining, Valsalva maneuver, or lumbar punctures.[3,4] Steroids, as previously noted in several case reports, can cause sudden neurological worsening, possibly secondary to an increase in venous hypertension, fluid shift, and change in oncotic pressure in the intravenous compartments.[5-7]In sDAVF, the epidural pressure slowly increases over time, leaving the patient’s spinal cord at a tipping point. A dose of steroids (oral/intravenous) results in a shift of oncotic balance with altered renal dynamics, subsequent water reabsorption, and shunting of blood in the venous circulation, worsening cord edema and ischemia, thus explaining the sudden deterioration of the neurological status.
MaterIals and Methods:
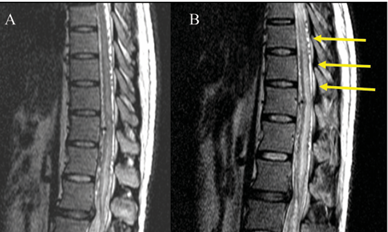
This study involved a retrospective analysis of prospectively collected data from patients diagnosed with sDAVF (type-1) from January 2001 to January 2020. All patients who underwent microsurgical disconnection of an angiographically proven sDAVF during the study period were included in the study. We excluded sDAVF patients treated by endovascular means. We also excluded patients undergoing a revision procedure. Patient consent was obtained for the purpose of the study with due care to maintain his/her privacy. We reviewed outpatient charts, inpatient charts, operation records, magnetic resonance imaging (MRI) scans, and spinal angiograms of these patients during the study period. Age, sex, duration of symptoms, comorbid conditions at the time of admission, sensory/ motor/bladder involvement, pre-intervention Nurick grade (NG),[9] modified Aminoff–Logue’s score (mALS),[10] imaging findings, and post-intervention NG were tabulated and analyzed. The dose of steroid administered, the timing of neurological deterioration, if any, in relation to the administration of steroids and surgery, and the postoperative outcomes in this specific subset of patients were statistically analyzed. The history of any acute neurological worsening before admission was also documented. The MR imaging features during the time of deterioration (wherever available) were also studied. All patients underwent MR imaging of the thoracolumbar (TL) spine with whole spine screening. We diagnosed sDAVF by the presence of T2-weighted hyperintensity within the cord and multiple flow voids in the subarachnoid space. The length of cord edema was measured in each MR image using the number of vertebral segments involved. Thin T2W coronal cuts were used to further identify the level of fistula, once the flow voids were identified on the sagittal images. All patients also underwent preoperative spinal angiograms [Figure 1] to confirm the diagnosis and ascertain the level of the sDAVF. The presence and location of the sDAVF were confirmed and agreed upon by all the authors. When the patients developed any acute preoperative neurological worsening after admission, an MRI of the spine was obtained whenever feasible. This imaging was examined for any new or increased T2W cord changes or bleeds
Steroid protocol
It is our institutional protocol to use dexamethasone perioperatively for intradural spine procedures to reduce the risks of cord edema. We prefer to use dexamethasone over other agents in view of its better cerebrospinal fluid pharmacokinetics.[11] The higher free plasma levels communication. Functional disability assessment was done using the modified Aminoff–Logue score (mALS) and NG of patients both before surgery and at the most recent follow-up. Improvement or deterioration of the neurological status of patients is determined by the change in NG pre- and post-intervention as measured by Nurick recovery rate (NRR). The NRR was estimated as (Preop NG – Follow-up NG)/Preop NG × 100
Statistical methods
Data were entered into a spreadsheet. Descriptive statistics were performed using percentages for categorical variables and median/mean for continuous variables. Statistical analysis was performed using Microsoft Excel (Microsoft Corp., Redmond, Washington, USA) and GraphPad software (Dotmatics, Boston, MA, USA). Univariate analysis for risk factors was performed using the chi-square test for categorical variables and the unpaired t-test for continuous variables. A P value of <0.05 was considered significant.
Results
Seven of the 62 sDAVF patients (11.3%) who underwent microsurgical excision experienced an acute neurological deterioration upon admission to our hospital [Figure 2], while 55 had no neurological worsening. All seven patients were male, and their ages varied from 35 to 73 years, with a mean age of 54.7 years ± 12.5 [Table 1]. The average length of symptoms before surgery was 15.7 months ± 29.1 (median: 12 months, range: 3–60 months). We observed that progressive myelopathy, the most common clinical syndrome at the time of presentation, was present in 93.4% of our patients. In total, 86% of our patients had bladder involvement. Furthermore,